Pseudomonas aeruginosa possesses multiple mechanisms of antibiotic resistance, leading to high morbidity and mortality rates. It may result in complex infections and dangerous septic cases in critically ill patients.
In a recent study, researchers from the University of Cologne, Cologne University Hospital, Helmholtz Center for Infection Research, and Hamburg University Hospital isolated antibodies from immune cells of chronic disease patients. These antibodies show potential as a novel approach to treating both acute and chronic infections caused by Pseudomonas aeruginosa. The study, titled “Discovery of highly neutralizing human antibodies targeting Pseudomonas aeruginosa,” was published online in the Cell journal on November 1, 2023.
Antibiotic-resistant bacteria pose a significant global health concern, impacting not only infected individuals but also our healthcare systems. Infections with Pseudomonas aeruginosa, particularly challenging due to its diverse resistance mechanisms, often lead to persistent colonization, resulting in complicated lung infections and progressive tissue damage, posing a threat to human health.
With standard treatments becoming less effective, patients often resort to last-resort antibiotics for infection treatment. Therefore, there is an urgent need for new therapeutic drugs to ensure effective treatment of multidrug-resistant pathogens like Pseudomonas aeruginosa.
In this new study, the researchers investigated whether the method of isolating broadly human neutralizing human antibodies, successful in treating viral infections, could also be applied to developing new therapies for bacterial infections. Dr. Alexander Simonis, co-first author and co-corresponding author from Cologne University Hospital, stated, “Many therapeutic antibodies used against viruses have been isolated and developed from infected individuals, convalescent individuals, or those vaccinated.”
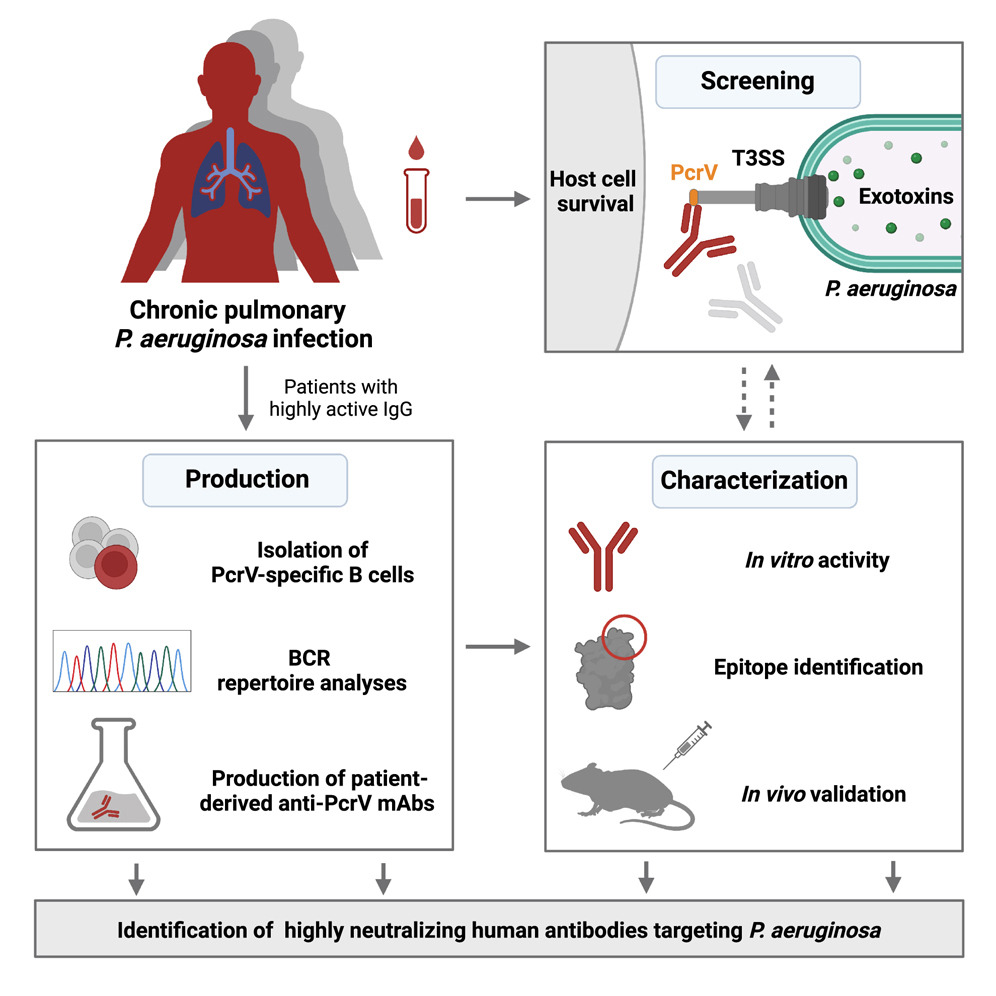
The authors isolated highly effective neutralizing antibodies targeting the pathogen from the immune cells of cystic fibrosis patients with long-term Pseudomonas aeruginosa infections. These antibodies can block a crucial virulence factor of the bacteria known as the type III secretion system, which plays a significant role in severe Pseudomonas aeruginosa infections.
Through extensive experiments using cell cultures and animal models, the researchers confirmed that these newly developed antibodies are as effective as traditional antibiotics. However, as the activity of these antibodies is unrelated to the mechanism and resistance of antibiotics, these so-called “pathoblockers” can also act against highly resistant bacteria compared to many traditional antibiotics.
Dr. Jan Rybniker, co-corresponding author from Cologne University Hospital, summarized, “These findings and experimental methods can be applied to other bacterial pathogens, making it a promising new approach for treating multidrug-resistant bacterial infections.”
The authors plan to further develop these antibodies for testing in clinical trials. In the long term, they intend to incorporate these antibodies as part of a new treatment method, especially in cases of acute and severe infections caused by Pseudomonas aeruginosa. According to their statement, these anti-Pseudomonas aeruginosa antibodies can also protect patients at an increased infection risk, particularly those in intensive care units or cancer patients, through passive immunity.