According to a study recently published in Cancer Research by researchers and colleagues at the Belvich Institute of Biomedicine at the University of Barcelona, a large number of replicated chromosome regions are linked to the resistance of cancer cells to chemotherapeutic drugs. The study was led by Eva González-Suárez, head of the IDIBELL Transformation and transfer Group.
Despite its’ side effects, chemotherapy is still the most effective treatment against cancer. One of the most extensive drugs in chemotherapy and one of the topics of this study is docetaxel, a chemotherapeutic drug that prevents tumor cell division. The study focused on the most aggressive breast cancer subtype: triple negative breast cancer (TNBC). This subgroup is characterized by strong heterogeneity (which is why there is currently no targeted treatment for it) and is usually associated with a poor prognosis. Although such patients initially respond well to chemotherapy, they tend to develop drug resistance during treatment. One of the challenges facing oncologists is to choose the right chemotherapeutic drugs for the benefit of triple negative breast cancer patients, and this choice is random in most cases.
To carry out the study, the scientists studied a patient-derived xenotransplantation model (PDXs). These PDXs are animal models (mice) that have been transplanted with cancer cells from patients, so this tumor model is more representative than traditional cell culture. These models can be used to test the effectiveness of drugs, or to study the process of chemotherapy-that is, to understand how tumor cells respond to treatment.
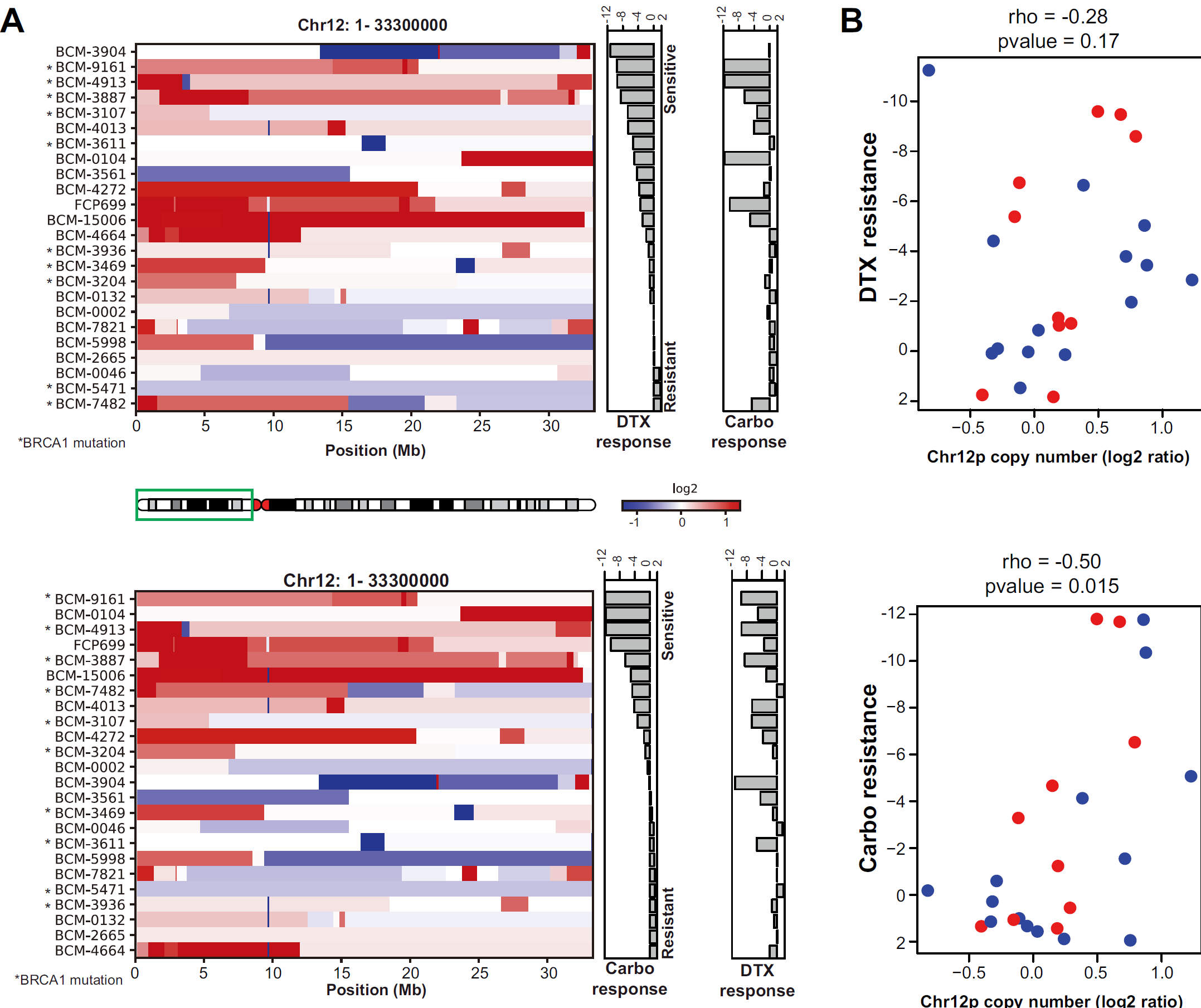
The researchers analyzed the effects of docetaxel on TNBC PDXs and found that resistance to docetaxel occurred during treatment. The genomes of tumors sensitive to docetaxel were compared with those of corresponding tumors that developed resistance after continuous drug exposure. They found that in tumors resistant to docetaxel, the number of copies of a region of chromosome 12, known as chr12p, increased, even after short-term treatment with docetaxel. These results suggest that subsets of tumor cells resistant to docetaxel exist in the tumor and survive.
In addition, the researchers found that the docetaxel-resistant subgroup was very sensitive to another chemotherapeutic drug, carboplatin, which is why Dr. Eva González-Suárez thinks it makes more sense to combine the two drugs in sequence.
“We associate this amplified chr12p chromosome region with the emergence of docetaxel resistance and carboplatin vulnerability,” Dr. Eva González-Suárez said. “We recommend that the copy number of chr12p be used as a biomarker to predict whether a patient’s tumor will develop docetaxel resistance; more importantly, when docetaxel resistance occurs, there should be an alternative drug to treat patients, that is, carboplatin.”
This finding may be the first description of biomarkers for the selection of chemotherapeutic drugs and the order of treatment beneficial to patients with TNBC.
Reference
1. Gomez-Miragaya, Jorge, et al. “Chromosome 12p amplification in triple-negative/BRCA1-mutated breast cancer associates with emergence of docetaxel resistance and carboplatin sensitivity.” Cancer research 79.16 (2019): 4258-4270.