Nowadays, immunotherapy has dramatically changed the care of cancer patients. In the case of patients with advanced melanoma, one of the most lethal cancers of human skin, the 5-year survival rate has increased from less than 10% to more than 50% because of the introduction of immunotherapy in 2011. However, immunotherapy is effective in only half of melanoma patients, and the other half who do not respond face a difficult future.
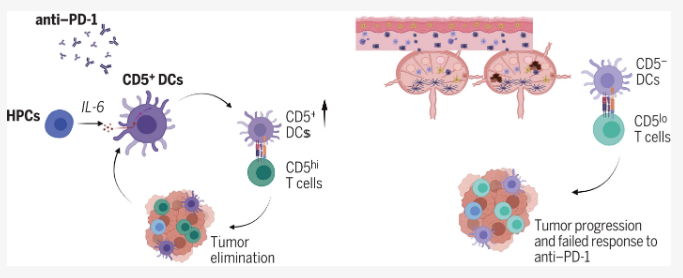
A study recently published in the international journal Science titled “CD5 expression by dendritic cells directs T cell immunity and sustains immunotherapy responses,” pointed out that the immune response of melanoma patients to immunotherapy is not always as high as it should be. In the study, scientists from the University of Washington School of Medicine and other institutions found that the difference in response to immunotherapy between patients may be related to immune cells called CD5+ dendritic cells, which carry a kind of specific protein called CD5 on their cell surface. Researchers stated that if the tumors contain more CD5+ dendritic cells, patients with melanoma or other cancers may live longer, while mice with dendritic cells lacking CD5 do not respond better to immunotherapy.
The findings probably suggest that complementary therapies designed to increase the number or activity of CD5+ dendritic cells may share the life-saving benefits of immunotherapy to more cancer patients. Dr. Eynav Klechevsky noted that although immunotherapy has revolutionized human cancer treatment today, but many cancer patients would not benefit from this therapy. The reason why some patients do not respond to certain immunotherapeutic forms is perhaps that their dendritic cell populations are dramatically reduced. Therefore, researchers are working to develop a novel immune-based approach to boost the activity of these CD5-expressing dendritic cells, aiming at enhancing patients’ responses to immunotherapy.
The immune system fights cancer by activating immune cells called T cells to recognize and kill tumor cells; in contrast, tumor cells manipulate the immune checkpoint system (a safeguard that prevents T cells from mistakenly attacking healthy cells) to interfere with the judgement of T cells. Immune checkpoint blockade therapy works by blocking the manipulation of tumor cells, thus allowing T cells to recognize and destroy the tumor cells. However, even with these treatments, the T cells in some patients’ bodies are still fail to function effectively. Therefore, Klechevsky and other researchers speculated that faulty dendritic cells of patients results in their no-response to immunotherapy. If T cells are likened to players on a soccer field, then dendritic cells are the coaches that get the players fired up and give them instructions; if without them, T cells would be suppressed and aimless.
By analyzing data from the Human Cancer Genome Database, the researchers found that patients with skin, lung, bone and soft tissue, breast, cervical cancers, etc., may be in better conditions if they have high levels of CD5+ dendritic cells in their tumors. After further analysis of human cells and mice, the researchers discovered that CD5+ dendritic cells may be necessary for T-cell activity to be effective against tumors. CD5+ dendritic cells from humans are very powerful in inducing T-cell activation and proliferation, while mice with tumors have such weak responses to immunotherapy that they may not be able to effectively reject tumors if CD5 is missing from their dendritic cells.
These findings show that the number of CD5+ dendritic cells in tumors could assist clinicians in assessing which patients would benefit most from immunotherapy. Additionally, increasing the activity or number of dendritic cells may potentially benefit more patients in immunotherapy treatment.
In conclusion, researcher Klechevsky pointed that we still don’t fully understand how immunotherapy works. The results of this study suggest that a lot of researches are required to improve the efficiency of these therapies. If we can find new ways to utilize these cells or expanding their levels in the patient’s body may help more patients. In summary, the results make clearly that CD5+ dendritic cells may be an essential component of optimal immune checkpoint blockade therapy for cancer treatments.
Reference
1. He, Mingyu, et al. “CD5 expression by dendritic cells directs T cell immunity and sustains immunotherapy responses.” Science 379.6633 (2023): eabg2752.