
Cancer Immunology
The field of cancer immunology delves into the complex relationship between the immune system and the processes of cancer formation, growth, and treatment. It centers on the potential of leveraging the immune system's natural mechanisms to combat cancer, leading to the development of innovative therapeutic strategies that have markedly improved patient outcomes. This exploration encompasses several critical areas, including the mechanisms of CAR-T cell therapy targets, the impact of cytokines on tumor development, the function of immune checkpoints in cancer evasion, and the role of cancer immunology in immune recognition. Each of these topics contributes to the broader understanding of how the immune system can be manipulated to target and destroy cancer cells, opening new avenues for treatment and research in oncology.
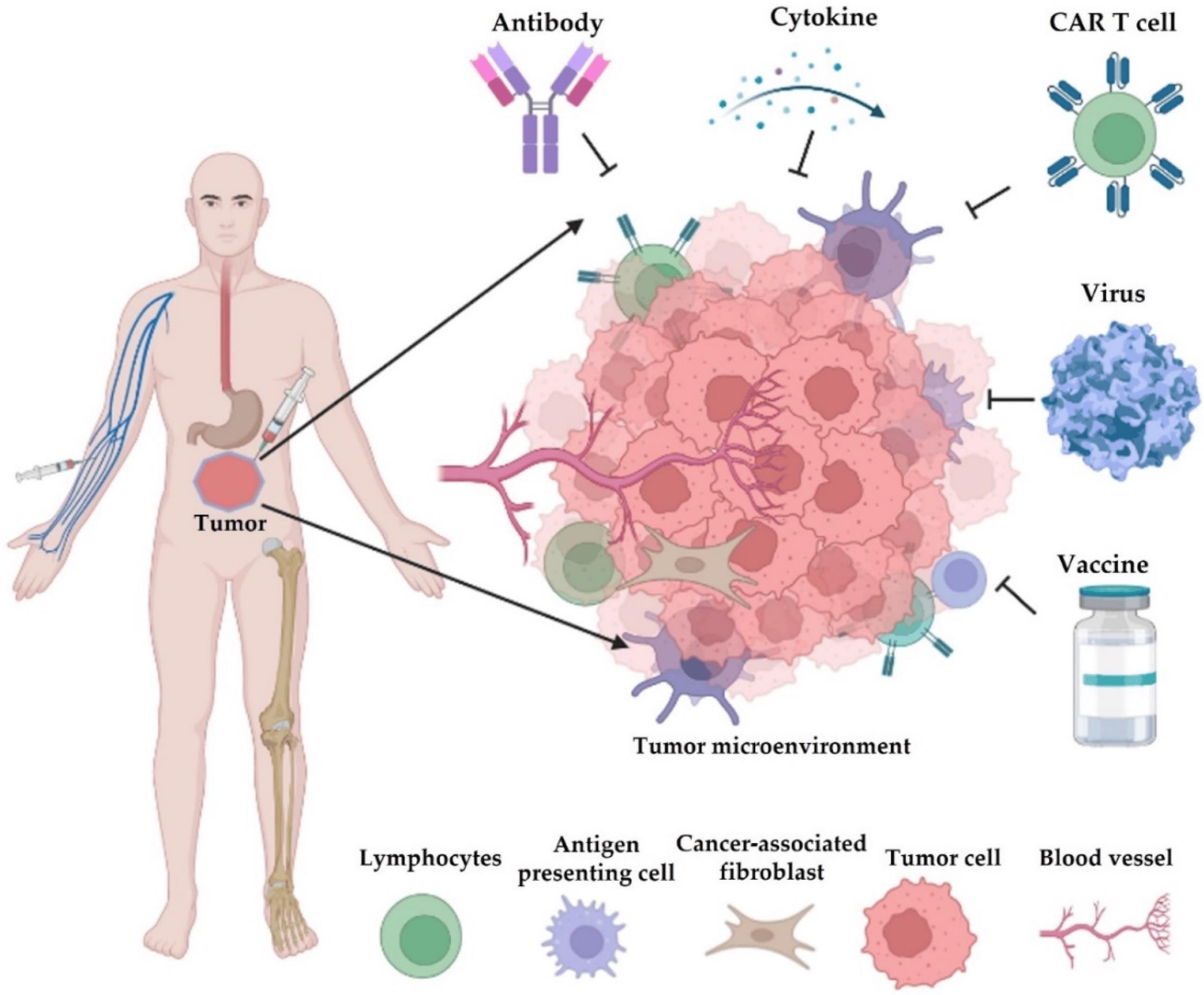 Figure 1 Different types of cancer immunotherapy. (Yang, 2018)
Figure 1 Different types of cancer immunotherapy. (Yang, 2018)
CAR-T Cell Therapy Targets
Chimeric antigen receptor (CAR) T-cell therapy represents a groundbreaking approach in cancer treatment, leveraging the body's immune system to fight cancer. This therapy involves genetically modifying a patient's T cells to express a CAR that targets specific antigens on the surface of cancer cells. Once these CAR-T cells are infused back into the patient, they recognize and kill cancer cells that express the targeted antigen. The selection of targets for CAR-T cell therapy is critical for its success. Ideal targets are antigens that are highly expressed on the surface of cancer cells but have limited or no expression on healthy cells to minimize off-target effects. For instance, in hematologic malignancies, CD19, a protein expressed on the surface of B cells, has been a successful target for CAR-T cell therapy, leading to significant remissions in patients with relapsed or refractory B-cell acute lymphoblastic leukemia (ALL) and other B-cell malignancies. Researchers are continuously identifying and validating new targets, such as BCMA (B-cell maturation antigen) in multiple myeloma, to expand the applicability of CAR-T cell therapy to other types of cancer.
Cytokines in Tumorigenesis
Cytokines are small proteins crucial for cell signaling in the immune system. They play a dual role in cancer, promoting or inhibiting tumor growth and progression. The tumor microenvironment, which includes cancer cells, immune cells, and other cells in the surrounding tissue, is rich in cytokines. These molecules can influence tumorigenesis through various mechanisms, including promoting inflammation, facilitating tumor cell proliferation and survival, inducing angiogenesis (formation of new blood vessels to supply the tumor with nutrients and oxygen), and modulating the immune response to cancer. For example, pro-inflammatory cytokines like TNF-α and IL-6 can contribute to tumorigenesis by promoting chronic inflammation, a known risk factor for several types of cancer. Conversely, cytokines such as IFN-γ and IL-12 have anti-tumor effects by enhancing the immune system's ability to recognize and destroy cancer cells. Understanding the complex role of cytokines in cancer is essential for developing therapies that can modulate their activity to treat cancer effectively.
Immune Checkpoints
Immune checkpoints are regulatory pathways in the immune system that help maintain self-tolerance and modulate the duration and amplitude of physiological immune responses. Cancer cells can exploit these pathways to evade immune detection and destruction. Two well-known immune checkpoint molecules are CTLA-4 (cytotoxic T-lymphocyte-associated protein 4) and PD-1 (programmed death-1), along with its ligand PD-L1. By expressing PD-L1, tumor cells can bind to PD-1 on T cells, effectively "turning off" the immune response against them. The development of immune checkpoint inhibitors, which are antibodies that block CTLA-4, PD-1, or PD-L1, has been a significant advance in cancer treatment. These drugs "release the brakes" on the immune system, enhancing its ability to recognize and kill cancer cells. Immune checkpoint inhibitors have shown remarkable success in treating a variety of cancers, including melanoma, non-small cell lung cancer, and renal cell carcinoma, among others. Ongoing research aims to identify additional immune checkpoints and develop new inhibitors to target them, potentially benefiting more patients with various types of cancer.
Tumor Antigens
Tumor antigens are molecules expressed on the surface of cancer cells that can be recognized by the immune system. These antigens can arise from various sources, including viral antigens in virus-associated cancers, cancer-testis antigens (expressed in various cancers but not in normal tissues except testis), differentiation antigens (associated with the differentiation state of the cancer cell), and neoantigens (resulting from tumor-specific mutations). The identification and characterization of tumor antigens have been crucial for developing cancer vaccines and other immunotherapies. For instance, therapeutic cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells expressing specific antigens. Similarly, neoantigens, which are unique to each patient's tumor, have emerged as promising targets for personalized cancer vaccines and T-cell therapies, offering the potential for highly specific and effective treatments.
- Yang, Ming, et al. "Cancer immunotherapy and delivery system: An update." Pharmaceutics 14.8 (2022): 1630.
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.