
Allograft Rejection Overview
Allograft rejection is the consequence of the recipient's alloimmune response to non-self antigens expressed by donor tissues. There are three major types of allograft rejection: hyperacute, acute, and chronic rejection. The first one, hyperacute rejection occurs within minutes and hours after transplantation and is caused via the presence of preexisting antidonor antibodies in the recipient blood. The kidney and heart are most susceptible to this condition, the liver is relatively resistant. The second one, acute rejection occurs within the first weeks or several months after transplantation and usually affects every transplanted organ to some different degree. Acute rejection is caused via the mismatch in highly polymorphic human leukocyte antigens (HLA) and is mediated primarily by T cells. They produce cytokines upon activation and recruit inflammatory cells eventually leading to necrosis of graft tissue. The third one, chronic rejection is probably caused via multiple factors: antibodies as well as lymphocytes. Chronic rejection develops within months to years after transplantation and is the main cause of long-term graft loss. The major feature of chronic rejection is accelerated arteriosclerosis or progressive luminal narrowing of graft vessels (vasculopathy or graft vascular disease (GVD)) often accompanied by graft tissue (parenchymal) fibrosis. These, in turn, lead to ischemia, cell death, and graft failure (Kloc, 2014).
Overview of allograft rejection pathways
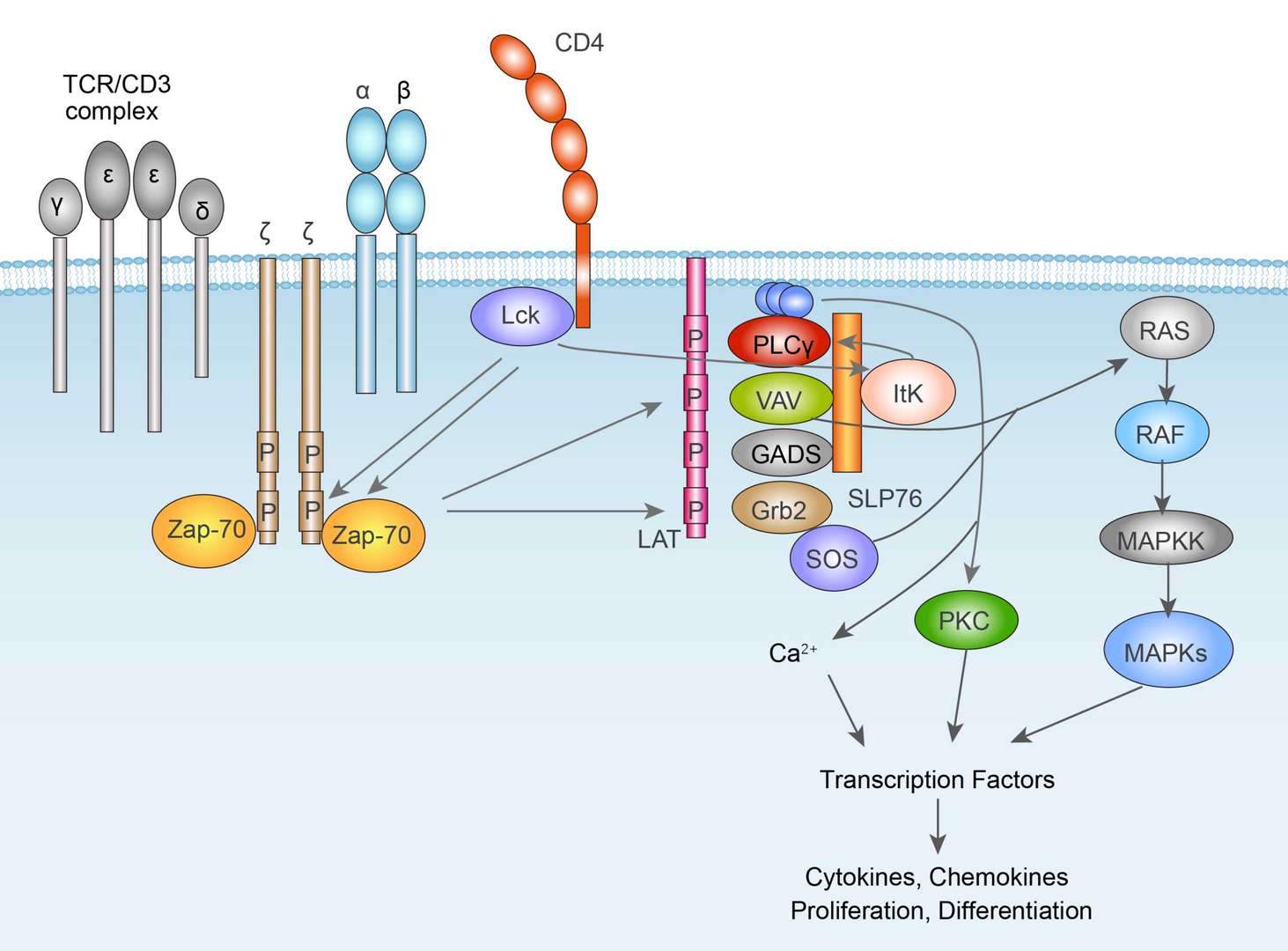
Main Signaling Pathways in Allograft Rejection
Diagnosis of Allograft Rejection
Hyperacute rejection occurs in a few minutes after the transplant when the antigens are completely unmatched. Diagnosis of acute rejection relies on clinical data and laboratory data, such as blood or even tissue biopsy. The laboratory pathologist generally seeks three major histological signs: (1) infiltrating T cells, possible accompanied by infiltrating eosinophils, plasma cells, and neutrophils, particularly in telltale ratios, (2) structural compromise of tissue anatomy, varying via tissue type transplanted, and (3) injury within blood vessels. Besides that, doctors also observe patient signs and symptoms to check whether patients are in acute rejection. To diagnose chronic rejection, it is again generally made by biopsy of the organ in question. Different organs have a different degree of damage from mild to severe. Chronic rejection occurs in heart grafts, it quickly develops "hardening of the arteries". Kidneys within chronic rejection have fibrosis (scarring) and damage to the microscopic blood vessels among the substance of the kidney. For livers, chronic rejection can result in a decreased number of bile ducts on biopsy. This is called as the "vanishing bile duct syndrome". Transplanted lungs with chronic rejection are said to have "bronchiolitis obliterans", a scarring problem in the substance of the lung.
Targeted Therapy for Allograft Rejection
Hyperacute rejection within minutes after the transplant, and so treatment must be immediate: removal of the tissue. Acute rejection is treated by one or several of a few strategies. Chronic rejection is commonly considered irreversible and poorly amenable to treatment. In terms of the targeted therapy, antibody specific to select immune components can be added to immunosuppressive therapy. The monoclonal anti-T cell antibody Muromonab-CD3, is an immunosuppressant drug given to reduce acute rejection in patients with organ transplants. It is a monoclonal antibody targeted the CD3 receptor. Other antibody drugs include basiliximab (used to prevent rejection in organ transplantation, especially in kidney transplants), daclizumab, which are monoclonal anti-IL-2Rα receptor antibodies; anti-thymocyte globulin (ATG- an infusion of horse or rabbit-derived antibodies against human T cells, which is used in the prevention and treatment of acute rejection in organ transplantation and therapy of aplastic anemia), anti-lymphocyte globulin (ALG-an infusion of animal- antibodies against human T cells) which is used in the treatment of acute rejection in organ transplantation), and are polyclonal anti-T-cell antibodies; as well as rituximab, a monoclonal anti-CD20 antibody.
Reference
- Kloc, M.; Ghobrial, R. M. (2014). Chronic allograft rejection: a significant hurdle to transplant success. Burns & trauma. 2014, 2(1): 3-10.
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
 TCR Signaling Pathway
TCR Signaling Pathway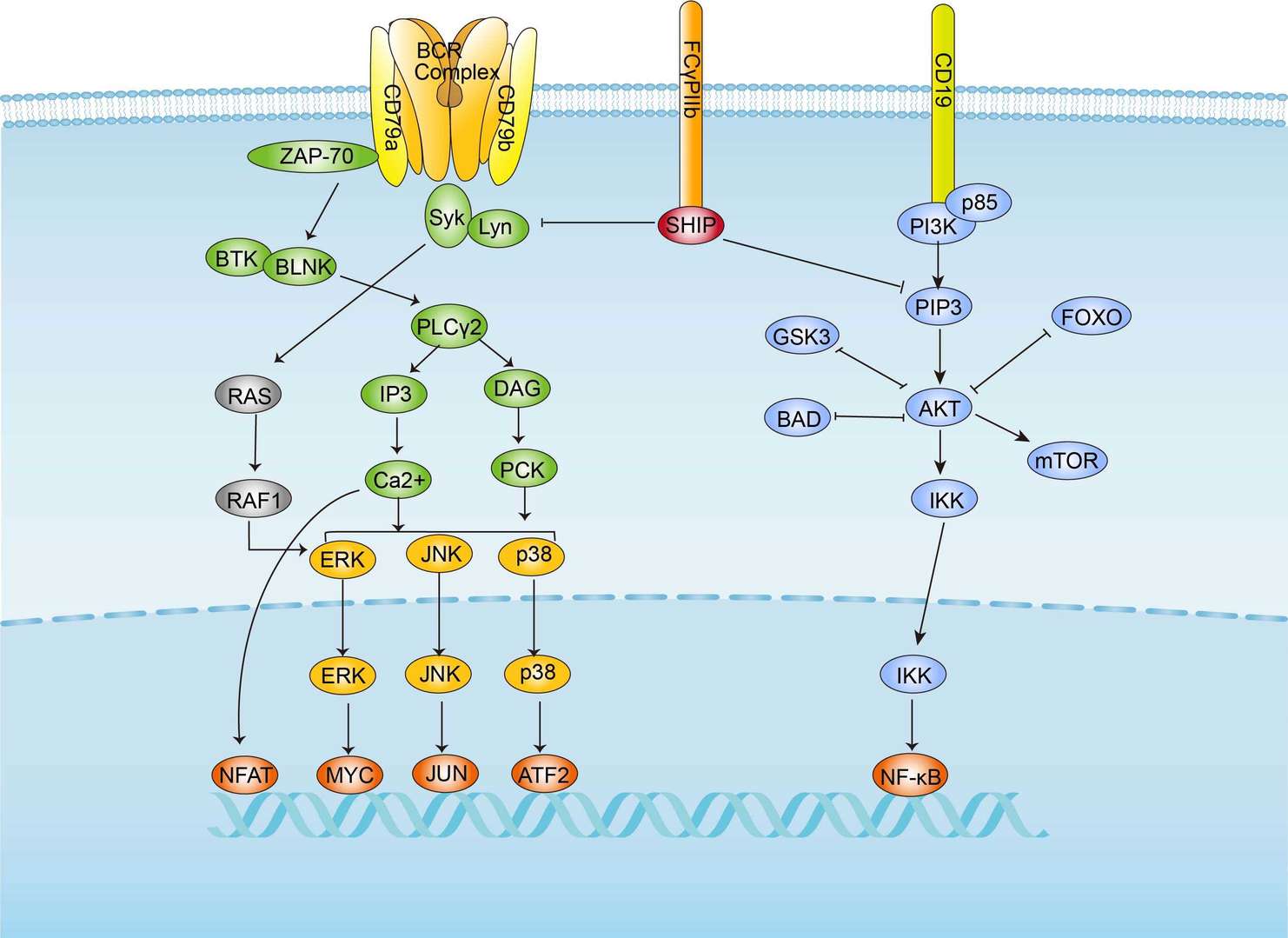 BCR Signaling Pathway
BCR Signaling Pathway