
Cushing Syndrome Overview
Introduction of Cushing Syndrome
Cushing syndrome occurs when the body is exposed to high levels of the hormone cortisol over a long period of time. Cortisol is produced in the adrenal glands and plays an important role in the body. For example, cortisol can regulate blood pressure, decreases inflammation, and keeps heart and blood vessels functioning normally. In some conditions, cortisol is called the “stress hormone” because it can help the body respond to stress. Moreover, it regulates the way people convert (metabolize) proteins, carbohydrates and fats in individuals’ diets into usable energy. However, when the level of cortisol is too high in the body, people possibly develop Cushing syndrome. Too much cortisol results in the hallmark signs of Cushing syndrome, including a fatty hump between patients’ shoulders, a rounded face, and pink or purple stretch marks on the skin. What’s more, Cushing syndrome can lead to high blood pressure, bone loss and, on occasion, type 2 diabetes. This type of Cushing syndrome is called “endogenous”. In general, endogenous Cushing syndrome occurs rarely. It is estimated that ranging from about 40 to 70 people out of every million.
The most common cause of Cushing syndrome is the long-term, high-dose use of glucocorticoids that are similar to cortisol. These medicines are usually utilized to treat other disorders, such as asthma NIH external link, rheumatoid arthritis NIH external link, and lupus NIH external link. Also, using glucocorticoids can suppress the immune system after an organ transplant to keep the body from rejecting the new organ. This type of Cushing syndrome is called “exogenous.” Except that, several types of tumors can cause the body to make excess cortisol, such as pituitary tumors, ectopic ACTH-producing tumors, adrenal tumors. Cushing syndrome most often affects adults, aged 30 to 50, but can also find in children. Furthermore, Cushing syndrome affects about three times as many women as men.
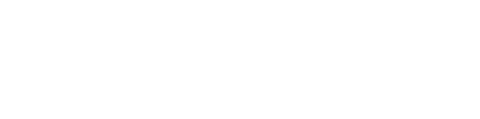
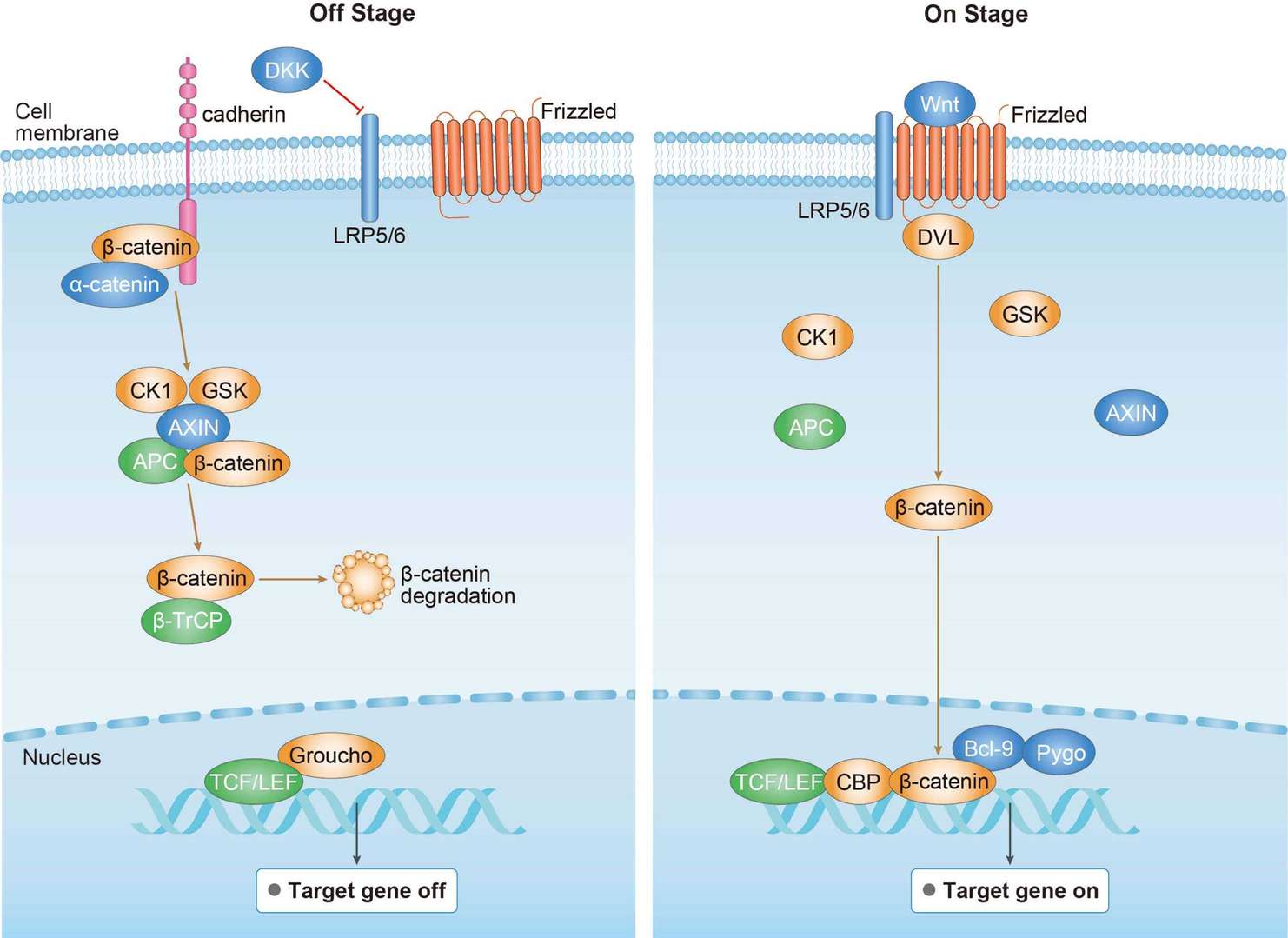
Overview of Cushing syndrome pathways
Main Signaling Pathways in Cushing Syndrome
Diagnosis of Cushing Syndrome
It is difficult to diagnose Cushing syndrome, particularly endogenous Cushing syndrome, because other conditions have the same signs and symptoms. Doctors will use a physical exam, looking for signs of Cushing syndrome. Candidates may suspect Cushing syndrome if they have signs, like the rounding of the face, a pad of fatty tissue between the shoulders and neck (buffalo hump), and thin skin with bruises and stretch marks. If they have been taking a corticosteroid medication for a long time, doctors may suspect that they have developed Cushing syndrome due to this medication. If individuals have not been using a corticosteroid medication, they need other diagnostic tests to help doctors to pinpoint the cause:
- Urine and blood tests. These tests measure hormone levels in the urine and blood and show whether the body is producing excessive cortisol. For the urine test, candidates may be asked to collect their urine over 24 hours. The samples of two tests will be sent to a lab to be analyzed for cortisol levels. Higher than normal cortisol levels suggest Cushing syndrome.
- Saliva test. Cortisol levels normally rise and fall throughout a day. If people without Cushing syndrome, levels of cortisol will drop significantly in the evening. This test measures the amount of cortisol in personal saliva in the late evening. Normally, cortisol production drops in the evening. However, people with Cushing syndrome, cortisol levels cannot drop.
- Dexamethasone suppression test (DST). DST is used to assess adrenal gland function by measuring how cortisol levels change in response to an injection of dexamethasone.
- Drugs for cravings: Naltrexone (ReVia) can help decrease the urge to have a drink. Acamprosate (Campral) may help for cravings.
- Imaging tests. Computerized tomography (CT) scans or magnetic resonance imaging (MRI) scans can provide images of candidate’s pituitary and adrenal glands to detect abnormalities, such as tumors.
Targeted Therapy for Cushing Syndrome
The best treatment for patients depends on the cause of the syndrome. If the cause of Cushing syndrome is long-term use of corticosteroid medications, the doctor can prescribe non-corticosteroid drugs, which will allow patients to decrease the dosage or eliminate the use of corticosteroid medications. If the cause of Cushing syndrome is a tumor, the doctor may recommend complete surgical removal. After the operation, patients need to take cortisol replacement medications to provide their body with the correct amount of cortisol. In most cases, patients eventually experience a return of normal adrenal hormone production, and doctors regularly decrease the replacement drugs. If the surgeon cannot remove a tumor, patients commonly prescribe radiation therapy.
Medications can be utilized to control cortisol production when surgery and radiation don't work. Also, doctors may recommend drug therapy before surgery to minimize surgical risk. Medications to control excessive production of cortisol at the adrenal gland include ketoconazole, mitotane (Lysodren) and metyrapone (Metopirone). Mifepristone (Korlym, Mifeprex) is approved for people with Cushing syndrome who have type 2 diabetes or glucose intolerance. The newest medication for Cushing syndrome is pasireotide (Signifor), and it works by reducing ACTH (Adrenocorticotropic Hormone) production from a pituitary tumor.
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
 Wnt Signaling Pathway
Wnt Signaling Pathway cAMP Signaling Pathway
cAMP Signaling Pathway