Autoimmune Thyroid Disease Overview
Autoimmune thyroid disease (AITD) is commonly observed together with other autoimmune diseases (Bliddal, 2017). AITDs, including Graves’ disease, Hashimoto’s thyroiditis (also known as chronic lymphocytic thyroiditis and Hashimoto’s disease), postpartum thyroiditis and atrophic autoimmune hypothyroidism, are complex organ specific autoimmune diseases that arise due to an interaction between environmental and genetic factors.
Symptoms of AITD may vary depending on the thyroid function, such as hyperthyroidism or hypothyroidism. For symptoms of hyperthyroidism include weight loss despite having a normal appetite, abnormal menstrual cycles, heat intolerance, increased sweating, palpitations, tremors, restlessness, increased bowel movements and nervousness. For symptoms of hypothyroidism include weight gain, weakness, dry skin, impaired memory, cold intolerance, abnormal menstrual cycles, hair loss, constipation and depression. Patients with both hyperthyroidism and hypothyroidism can experience severe fatigue. However, some patients with thyroid disease may have no clinical symptoms, or the symptoms can be so mild that they may be unnoticed. Graves’ disease can result in uncontrolled production of thyroid hormone and hyperthyroidism (increased thyroid function). Hashimoto’s thyroiditis characterized via loss of thyroid gland cells, which are responsible for the production and secretion of thyroid hormones, leading eventually to hypothyroidism (decreased thyroid function). Postpartum thyroiditis can happen soon after a woman gives birth and may reoccur after subsequent pregnancies; it usually presents with hyperthyroidism followed by hypothyroidism. Atrophic autoimmune hypothyroidism is a rare condition characterized by autoantibodies and functional hypothyroidism (also known as subclinical hypothyroidism). When patients are in AITDs, autoantibodies bind to the thyroid gland, resulting in inflammation, thyroid dysfunction and other clinical manifestations.
Overview of autoimmune thyroid disease pathways
Main Signaling Pathways in Morphine Addiction
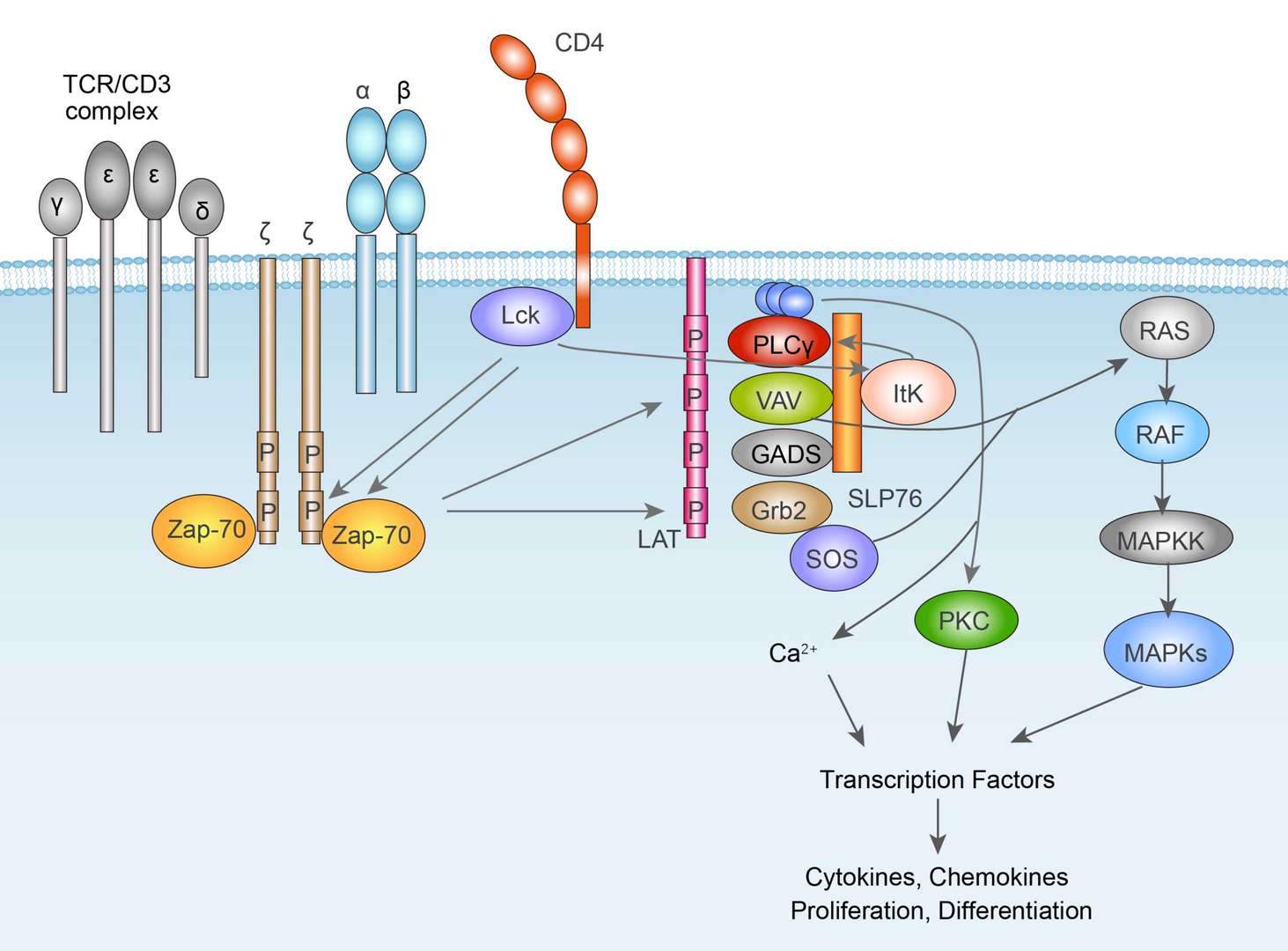 TCR Signaling Pathway
TCR Signaling Pathway
Diagnosis of Autoimmune Thyroid Disease
Diagnosis tests can be chosen depending on the presenting symptoms. Doctors may search for Thyroid peroxidase Antibodies (TPOAb) when patients have symptoms of hypothyroidism, or when patients will be started on a drug therapy associated with risks of developing hypothyroidism, such as lithium or Interferon alfa (Dayan, 1995). This antibody is related to Hashimoto's thyroiditis and Graves' disease. If the patient has symptoms of hyperthyroidism, doctors more likely ask patients for test about Thyroid stimulating hormone receptor Antibodies (TRAb), and monitor the effects of anti-thyroid therapy meanwhile, also associated with Graves' disease. Moreover, doctors may check Thyroglobulin Antibodies (TgAb) also, whenever a thyroglobulin test is performed to see if the antibody is interfering.
Targeted Therapy for Autoimmune Thyroid Disease
The main types of targeted therapy are currently small molecules and monoclonal antibodies. There are small molecule drugs treating AITDs. Therapies for Hashimoto's disease include observation or medications. Observation is recommended firstly if the thyroid gland is functioning normally. However, if Hashimoto's disease results in thyroid hormone deficiency, patients will need thyroid hormone replacement therapy. Under this condition, patients usually need use synthetic form of thyroxine (T4), which is levothyroxine. The treatment aim for Graves' disease is to stop the production of thyroid hormones. Some treatments include: propylthiouracil (PTU) and methimazole, which are anti-thyroid medications. PTU is a medication used to treat hyperthyroidism. Moreover, thiamazole, also known as methimazole, is a medication used to treat hyperthyroidism. Besides these, doctors recommend anti-thyroid medications interfere with the thyroid's use of iodine to produce hormones. These prescription medications include propylthiouracil and methimazole (Tapazole). Sometimes, patients need beta blockers, including Propranolol (Inderal), Atenolol (Tenormin), Metoprolol (Lopressor, Toprol-XL), Nadolol (Corgard).
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.


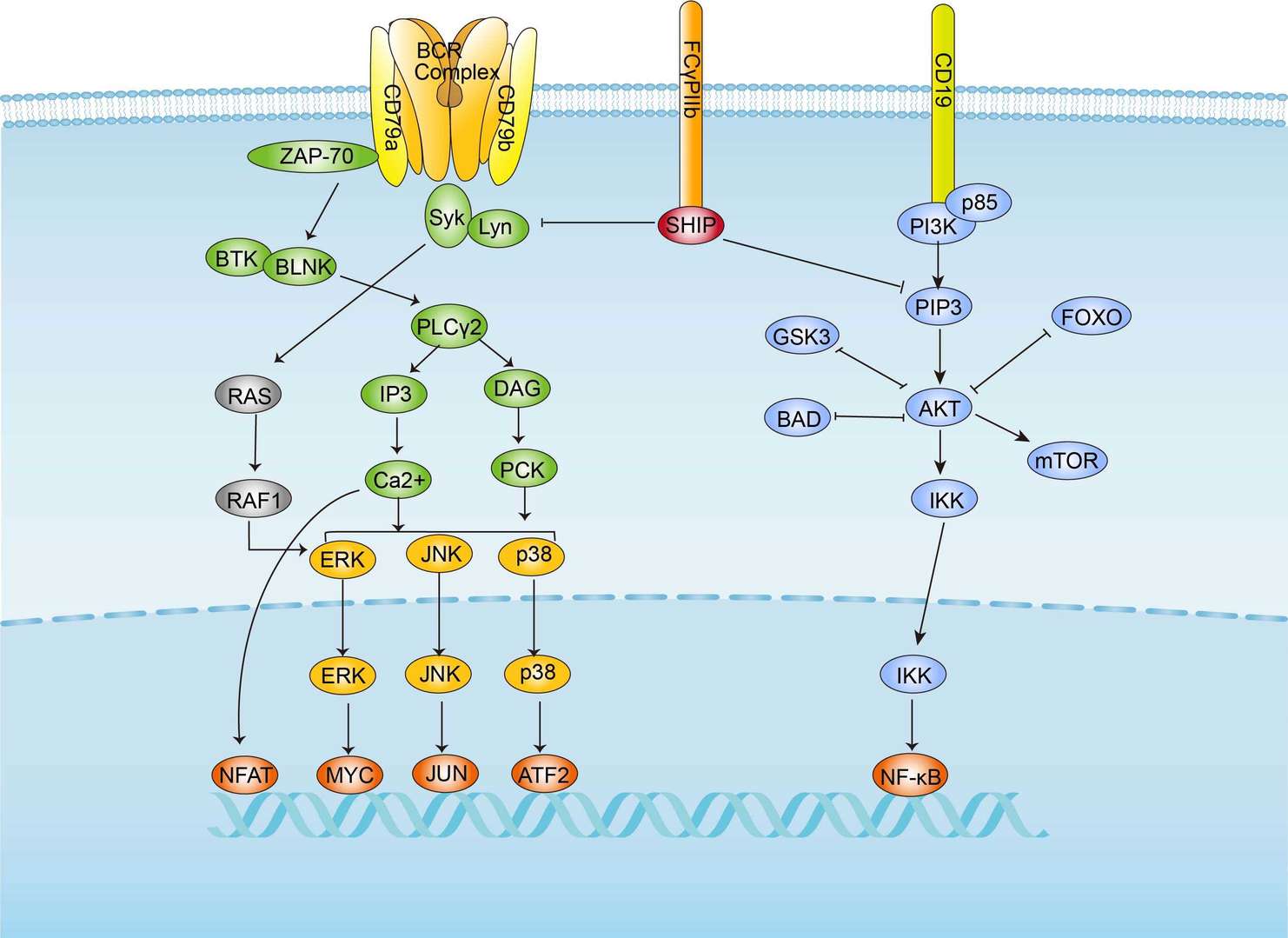 BCR Signaling Pathway
BCR Signaling Pathway