Systemic Lupus Erythematosus Overview
About Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is the most common type of lupus and autoimmune disease in which the immune system attacks its tissues, causing widespread inflammation and tissue damage in the affected organs. It influences the joints, skin, brain, lungs, kidneys, and blood vessels. Patients have symptoms, including fatigue, skin rashes, fevers, and pain or swelling in the joints. For some adults, having a period of SLE symptoms—called flares—possibly happen so often, sometimes even years apart, and go away at other times—called remission. However, other adults have SLE flares more frequently throughout their life. Besides that, sun sensitivity, oral ulcers, arthritis, lung problems, heart problems, kidney problems, seizures, psychosis, and blood cell and immunological abnormalities, these are all symptoms with SLE. The reasons for SLE are unknown, but are commonly thought to be linked to environmental, genetic, and hormonal factors. The seriousness of SLE can range from mild to life-threatening. So far, there has no cure for lupus, but medical interventions and lifestyle changes can help control disease conditions. SLE is an autoimmune disorder characterized via antibodies to nuclear and cytoplasmic antigens, multisystem inflammation, protean clinical manifestations, and a relapsing and remitting course. More than 90% of cases of SLE occur in women, frequently starting at childbearing age.
Overview of pathways in systemic lupus erythematosus
Main Signaling Pathways in Systemic Lupus Erythematosus
Diagnosis of Systemic Lupus Erythematosus
SLE may be difficult to diagnose, especially for the early stage, because early signs and symptoms are not specific. Currently, the diagnosis of SLE is based on characteristic clinical findings of the skin, joints, kidneys, and the central nervous system, as well as on serological parameters such as antinuclear antibodies (ANA), in particular, antibodies to dsDNA. Generally, doctors use the results of lab tests and clinical manifestations together to check whether patients have SLE.
- Clinical manifestations
- Lab tests
About clinical manifestations, cutaneous manifestations occur in about 75% of patients with SLE in the course of the disease, and are the first sign in a quarter of cases (Jimenez, 2004). The musculoskeletal system is involved in almost 90% of patients with SLE. In addition to myalgia and arthralgia, arthritis of small and large joints possibly occurs in patients (Fischer-Betz, 2005). Furthermore, tendovaginitis and synovitis can be detected via sonography and/or magnetic resonance imaging. Around 50% of patients with SLE develop renal involvement. Lupus nephritis is glomerular nephritis, typically with proteinuria and erythrocyturia (particularly dysmorphic erythrocytes) as well as erythrocyte cylinders in the urinary sediment.
Undergoing complete blood count may reveal leukopenia, mild anemia, and/or thrombocytopenia. Elevated serum creatinine can indicate renal dysfunction. Urinalysis with urine sediment can reveal hematuria, pyuria, proteinuria, and/or cellular casts. Serum protein electrophoresis can show a hypergammaglobulinemia that is suggestive of a systemic inflammatory process. These results of tests provide proof for doctors to indicate whether patients have SLE. In addition to the routine lab tests described above, there are several the following laboratory tests, which further diagnose SLE: antinuclear antibody (ANA, ideally via indirect immunofluorescence testing); anti-double-stranded DNA (anti-dsDNA); antiphospholipid antibodies, such as lupus anticoagulant (LA), immunoglobulin (Ig) G and IgM anticardiolipin (aCL) antibodies, and IgG and IgM anti-beta2-glycoprotein; C3 and C4 or CH50 complement levels; erythrocyte sedimentation rate (ESR) and/or C-reactive protein (CRP) levels; urine protein-to-creatinine ratio
Targeted Therapy for Systemic Lupus Erythematosus
Treatment for SLE depends on patients’ signs and symptoms. The medications, including small molecules and monoclonal antibodies, most commonly used include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as naproxen sodium (Aleve) and ibuprofen (Advil, Motrin IB, others), can be used to treat pain, swelling and fever associated with lupus. Stronger NSAIDs are available by prescription.
- Antimalarial drugs. This type of drug, such as hydroxychloroquine (Plaquenil), affects the immune system and can help decrease the risk of lupus flares.
- Corticosteroids. Prednisone and other types of corticosteroids can counter the inflammation of lupus. High doses of steroids such as methylprednisolone (A-Methapred, Medrol) are often utilized to control serious disease that involves the kidneys and brain.
- Immunosuppressants. Drugs that suppress the immune system are helpful in serious cases of lupus. For example, azathioprine (Imuran, Azasan), mycophenolate mofetil (CellCept) and methotrexate (Trexall).
- Biologics. Belimumab (Benlysta) administered intravenously, also reduces lupus symptoms in some patients. Rituximab (Rituxan) is beneficial in cases of resistant lupus.
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.


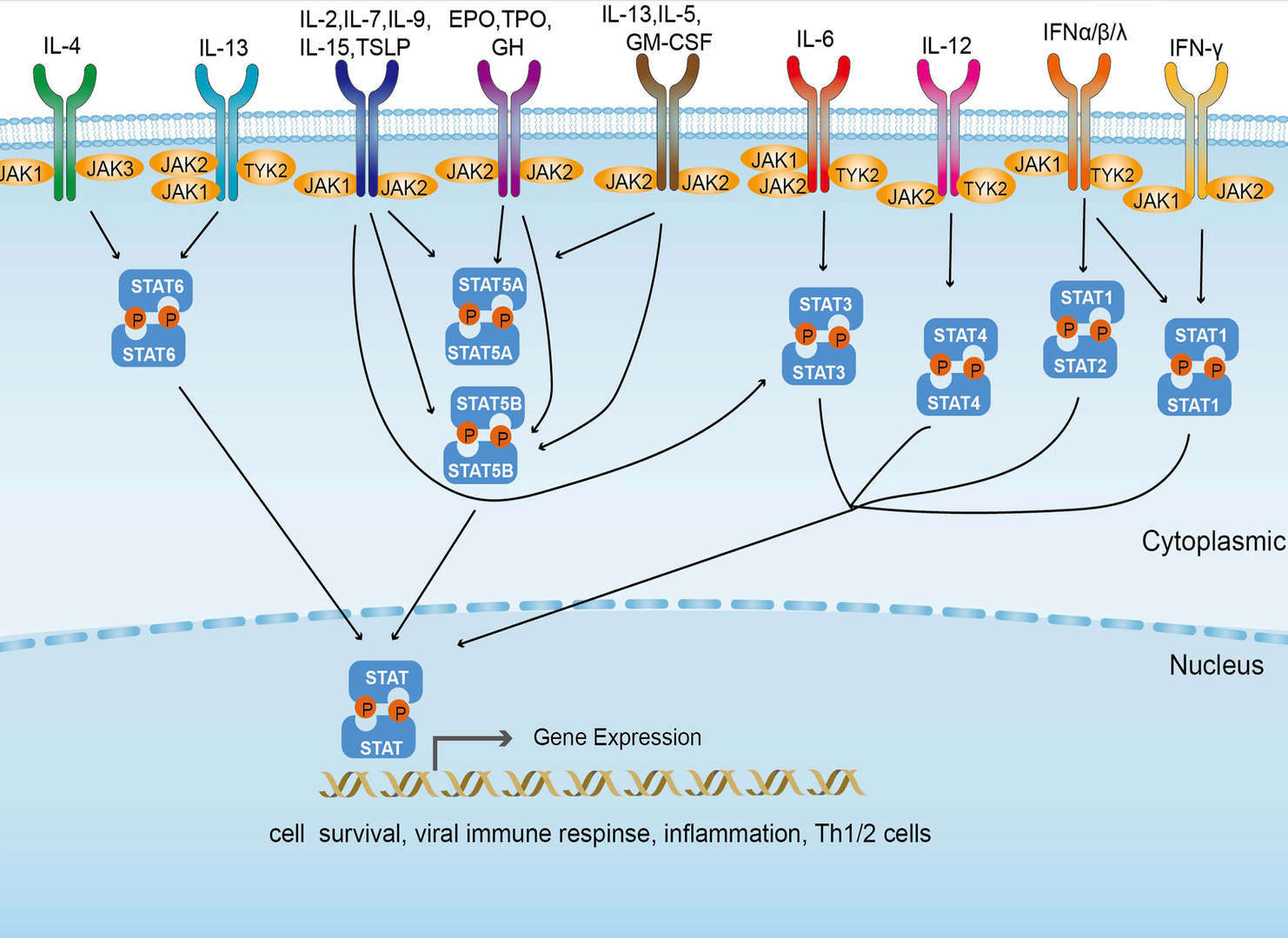 JAK-STAT Signaling Pathway
JAK-STAT Signaling Pathway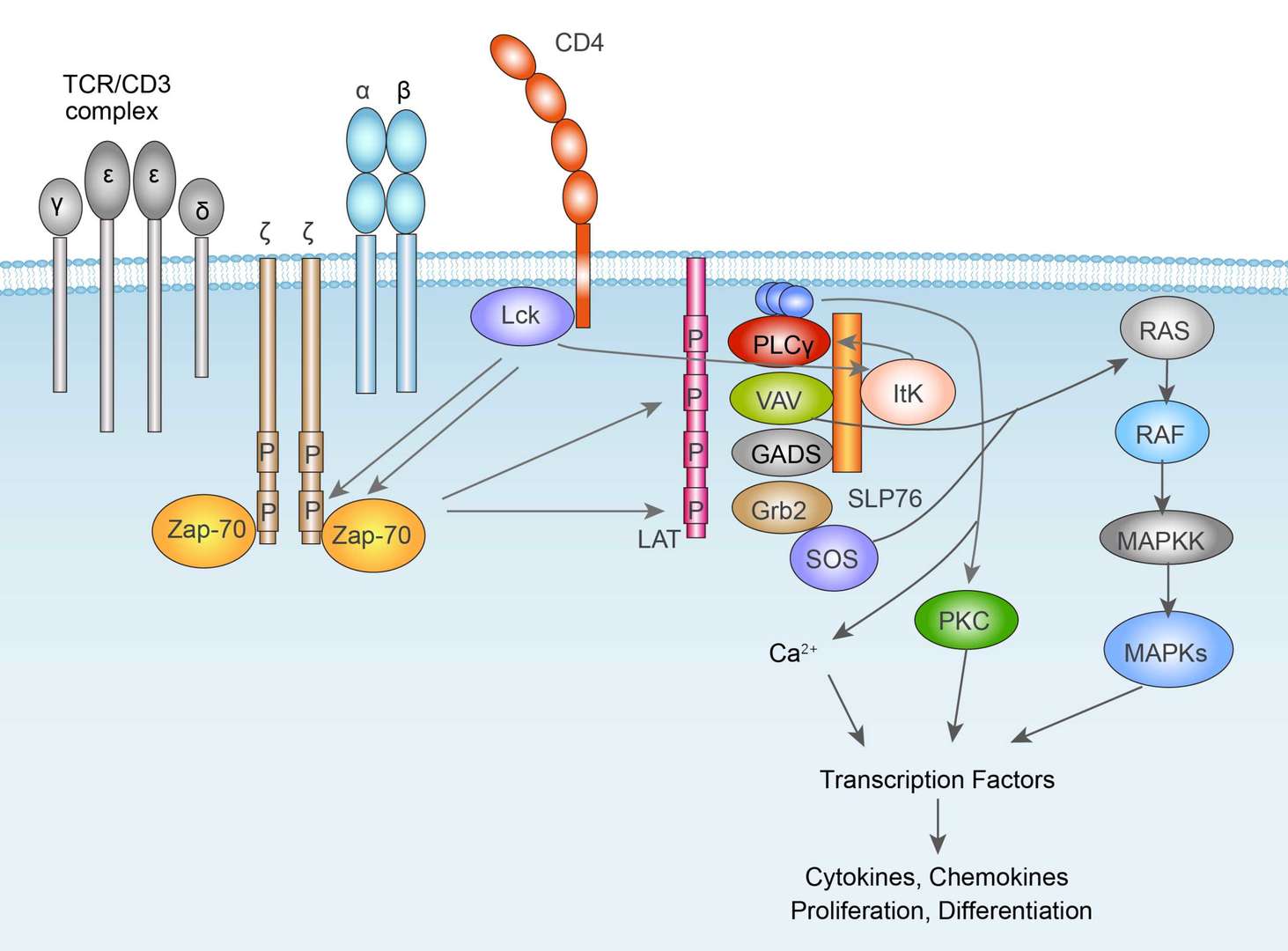 TCR Signaling Pathway
TCR Signaling Pathway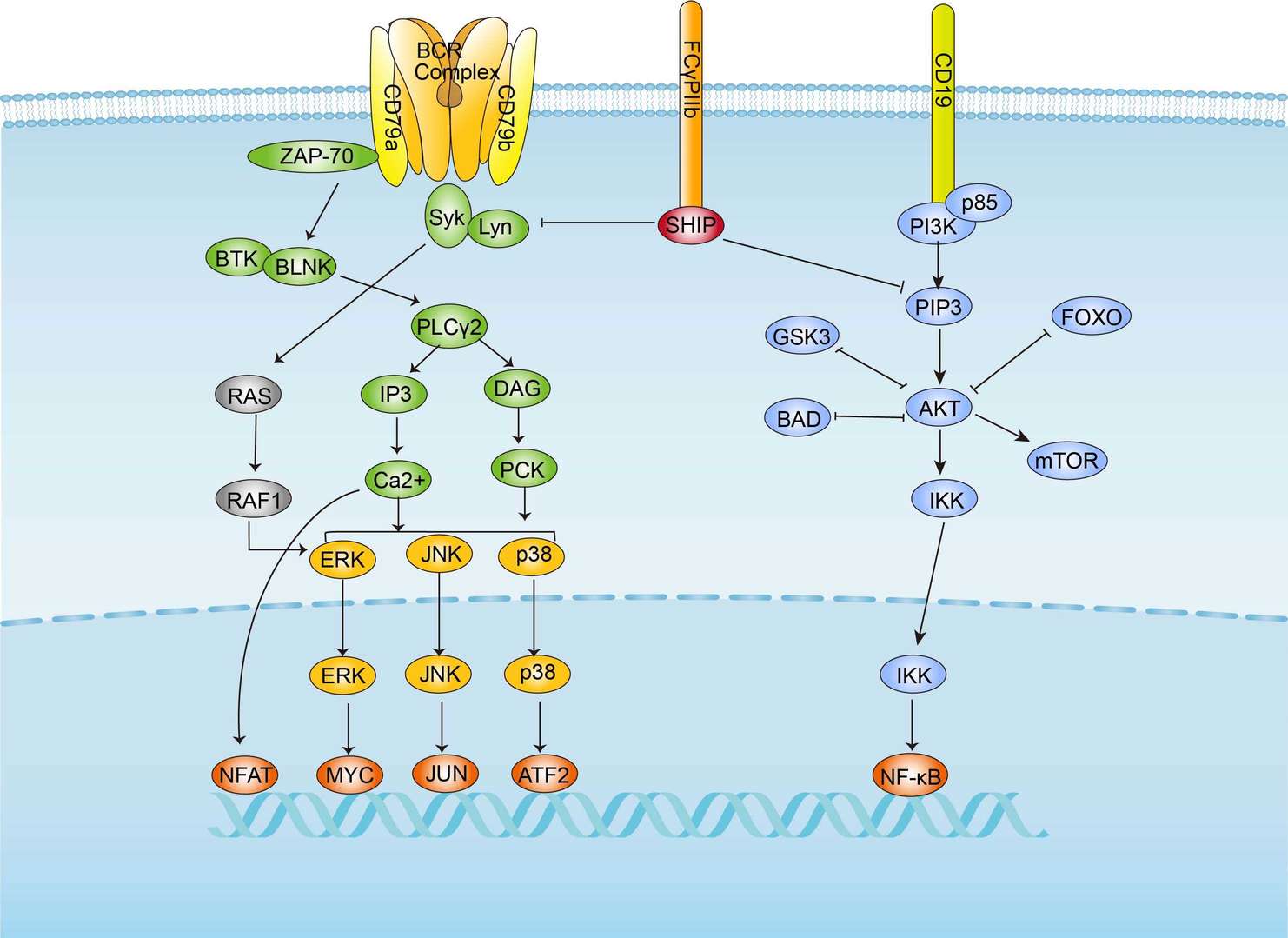 BCR Signaling Pathway
BCR Signaling Pathway