Type I Diabetes Mellitus Overview
About Type I Diabetes Mellitus
Type 1 diabetes mellitus, known as juvenile diabetes, is an autoimmune disease in which the body cannot make enough insulin to control blood sugar levels. This means it starts when the immune system attacks cells in the body. In this disease, the immune system destroys insulin-producing cells (beta cells) in the pancreas. This results in patients with little or no insulin. Without insulin, sugar accumulates in the bloodstream rather than entering the cells. As a result, the body cannot utilize this glucose for energy. In addition, the high levels of glucose that remain in the blood can result in excessive urination and dehydration, and damage tissues of the body. The cause of type 1 diabetes is unknown. However, it is believed to involve a combination of genetic and environmental factors. For example, whether having a family member with the condition. Type 1 diabetes mellitus makes up an estimated 5–10% of all diabetes cases. The number of people affected is unknown around the world, although it is estimated that about 80,000 children develop the disease each year.
Main Signaling Pathway in Type I Diabetes Mellitus
Type 1 diabetes mellitus is diagnosed via a combination of symptoms, age and blood tests. The blood tests include tests for sugar levels and other substances.
- First is the fasting plasma glucose (FPG) test. Blood is taken in the morning after fasting overnight. Blood sugar levels generally remain between 70-100 milligrams per deciliter (mg/dL). Patients will be diagnosed if the blood sugar level is 126 mg/dL or higher.
- Second is the oral glucose tolerance test (OGTT). Blood sugar is measured two hours after drinking 75g glucose. Patients will be diagnosed if the blood sugar level is 200 mg/dL or greater.
- Then the random blood glucose test. A blood sugar of 200 mg/dL or greater at any time of a day.
- Finally, hemoglobin A1C (glycohemoglobin). This tests the average glucose level over the prior two to three months. Diagnosed if the hemoglobin A1C level is 6.5% percent or greater.
Targeted Therapy for Type I Diabetes Mellitus
Several types of insulin are available for treating type 1 diabetes mellitus. Rapid-acting starts to work in about 15 minutes and peaks about 1 hour after patients take it and continue to work for 2-4 hours, such as insulin glulisine (Apidra), insulin lispro (Humalog) and insulin aspart (Novolog). Regular or short-acting gets to work in around 30 minutes and peaks between 2 and 3 hours and keeps working for 3-6 hours, such as Humulin R and Novolin R. Intermediate-acting won’t get into the bloodstream for 2-4 hours after patients are shot and peaks from 4 to 12 hours and works for 12-18 hours, such as insulin NPH (Novolin N, Humulin N). Long-acting takes several hours to get into patients and works about 24 hours, such as insulin glargine (Lantus, Toujeo Solostar), insulin detemir (Levemir) and insulin degludec (Tresiba).
Besides that, patients also need to eat a healthy diet, exercise regularly, and maintain a healthy weight. In daily life, patients need to monitor the blood sugar level all the time. This aim is to keep the blood sugar level as close to normal as possible to delay or stop complications. Generally, the goal is to keep the daytime blood sugar levels between 80 and 130 mg/dL (4.44 and 7.2 mmol/L) before meals and no higher than 180 mg/dL (10 mmol/L) two hours after meals.
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.


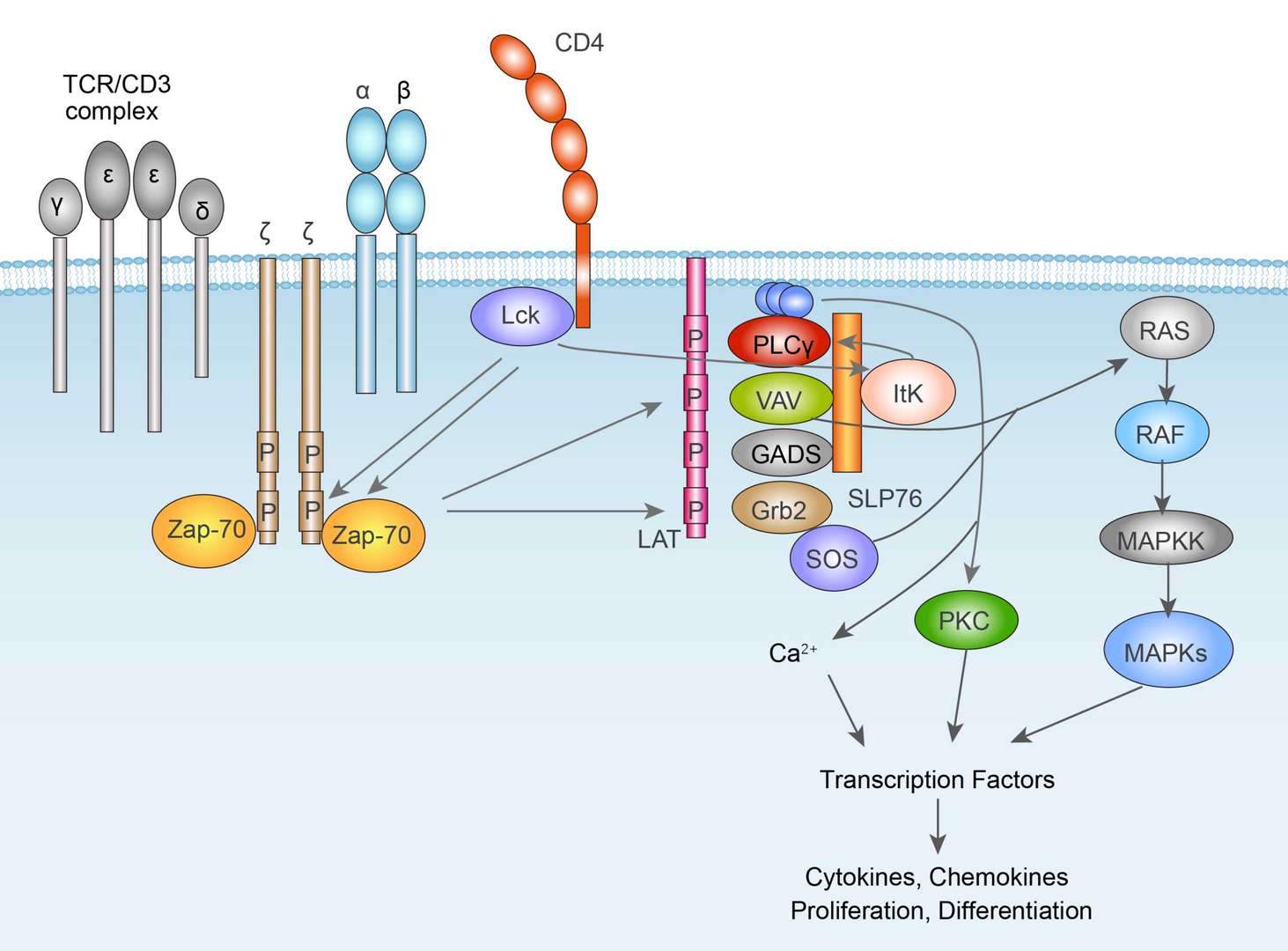 TCR Signaling Pathway
TCR Signaling Pathway