Primary Immunodeficiency Overview
Many diseases with various symptoms can result from mutations in immune system-related genes, the majority of which manifest as recurrent infections as a result of compromised immune function. This heterogeneous disease known as primary immunodeficiency disease (PID) can generally be divided into two categories: innate immune disease and adaptive immune disease. It poses a huge threat to human health because it is often accompanied by persistent infections and associated complications. Given the importance of PID for the prevention of many serious diseases, the diagnosis and treatment of PID have emerged as a significant medical research topic.
Overview of pathways in primary immunodeficiency
Main Signaling Pathways in Thyroid Cancer
Classification of PID
PIDs can be divided into the following two types based on the immune system's defective cells or tissues:
- Disorders of adaptive immunity. T cells may have genetic flaws that affect their ability to differentiate and develop, while B cells may also have flaws that affect their ability to produce antibodies. A combined immunodeficiency disease (CID) will typically develop as a result of T cell-associated gene deficiency because the production of antibodies also requires full T cell function.
- Disorders of innate immunity. The innate immune response, the first line defense against foreign invasions, can identify threats and induce inflammatory cascades to remove invading microorganisms from the physiological system. The inability of the innate system to recognize the pathogen delays the induction of the immune response and may exacerbate the infection. Any cell or protein defect involving an innate immune response may cause PID.
Clinical Presentation of PID
- T-cell and CID. The clinical manifestations of T-cell disease and CID will vary according to specific underlying defects in the adaptive immune response. Patients with specific T cell defects may manifest lymphopenia and neutropenia. Serious life-threatening CIDs are generally rare, and most CIDs will have associated common applications such as Wiskott-Aldrich syndrome, DiGeorge syndrome, ataxia-capillary vasodilation, as well as autoimmune and immune modulation abnormalities.
- B-cell immunodeficiencies. B cell defects are the most common type, accounting for approximately 50% of all PID cases, which are characterized by an increased sensitivity to respiratory infections of bacteria, especially Streptococcus pneumoniae and Haemophilus influenzae and in turn lead to a series of heterogeneous diseases. Patients usually develop relapses after 6 months, often with severe lung infections such as otitis media, sinusitis, and pneumonia. Diarrhea, fatigue, autoimmune manifestations, and sensorineural hearing loss are also common. Patients with humoral deficiency often have serum immunoglobulin levels that decrease or disappear and may have normal or elevated serum immunoglobulin levels but with abnormal functions.
- Innate immunodeficiencies. Congenital immunodeficiency diseases are usually accompanied by hard-to-eradicate infections. Typical symptoms of common phagocyte defects such as chronic granulomatous disease (CGD) are severe purulent bacterial and fungal infections of the skin, respiratory tract, and internal organs. Complement-deficient diseases are less common and tend to show systemic autoimmune diseases or recurrent infections similar to lupus erythematosus.
Treatment of PID
At present, treatment strategies for PID in the medical system are very complicated, most of which require immunologists with disease management expertise to formulate various aspects of coordination strategies. To lessen the frequency and severity of infections in patients with CID, it is typically necessary to treat diagnosed infections first. Severe CID is fatal and requires response to relative genetic defects. Hematopoietic stem cell transplantation can be used to re-establish the immune system, or gene therapy can be used to introduce functional genes to make up for the patient's own defects.
Ig injection is typically used to treat antibody shortage brought on by B cell defects, which, in most cases, necessitates long-term maintenance. It is divided into intravenous and subcutaneous injections, which can be selected according to the patient's habits and adverse reactions. Congenital immune deficiency mainly considers the prevention of infection. Repairing defects using foreign functional genes will also be a significant treatment strategy as gene therapy advances.
For research use only. Not intended for any clinical use.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.


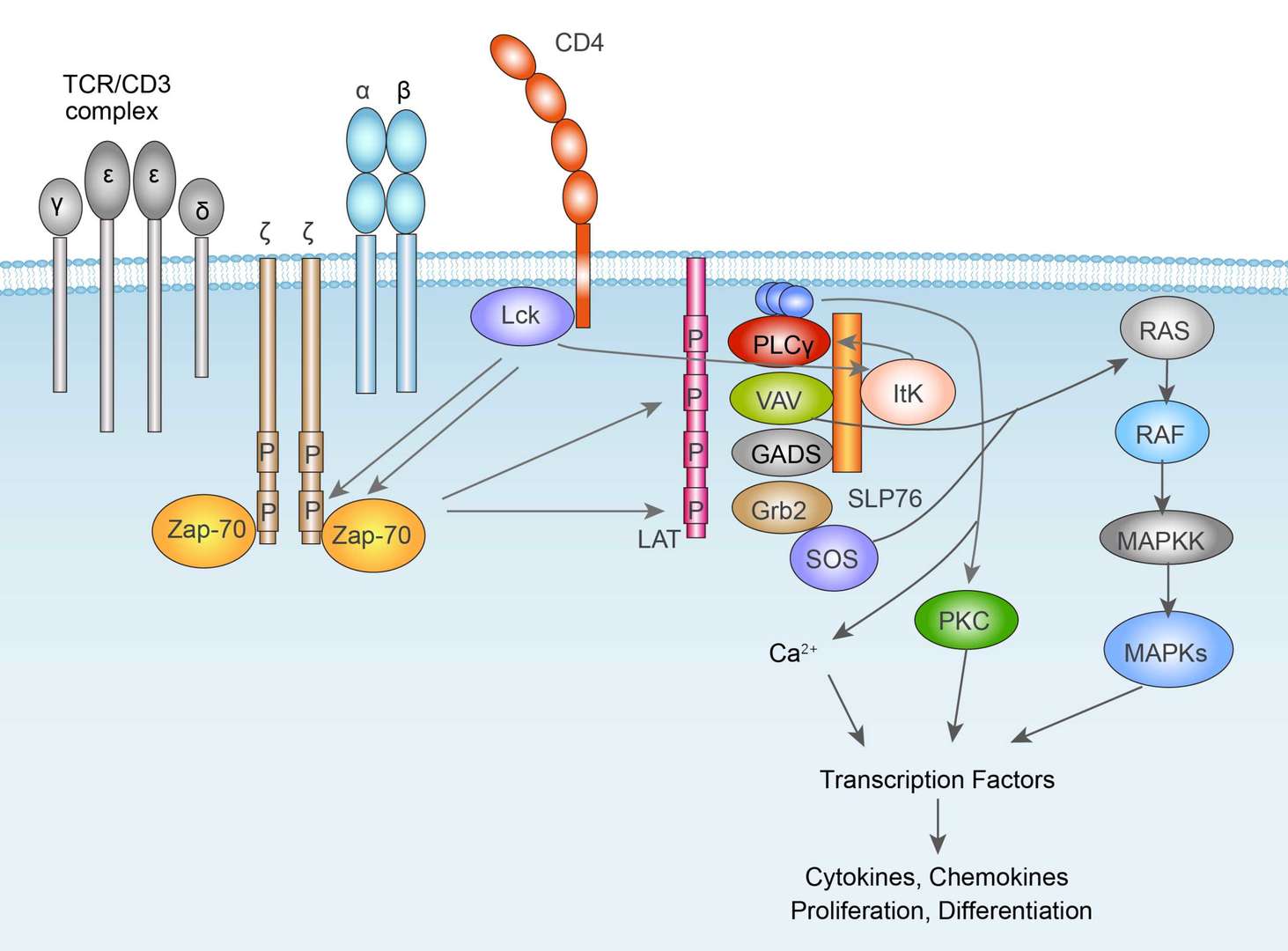 TCR Signaling Pathway
TCR Signaling Pathway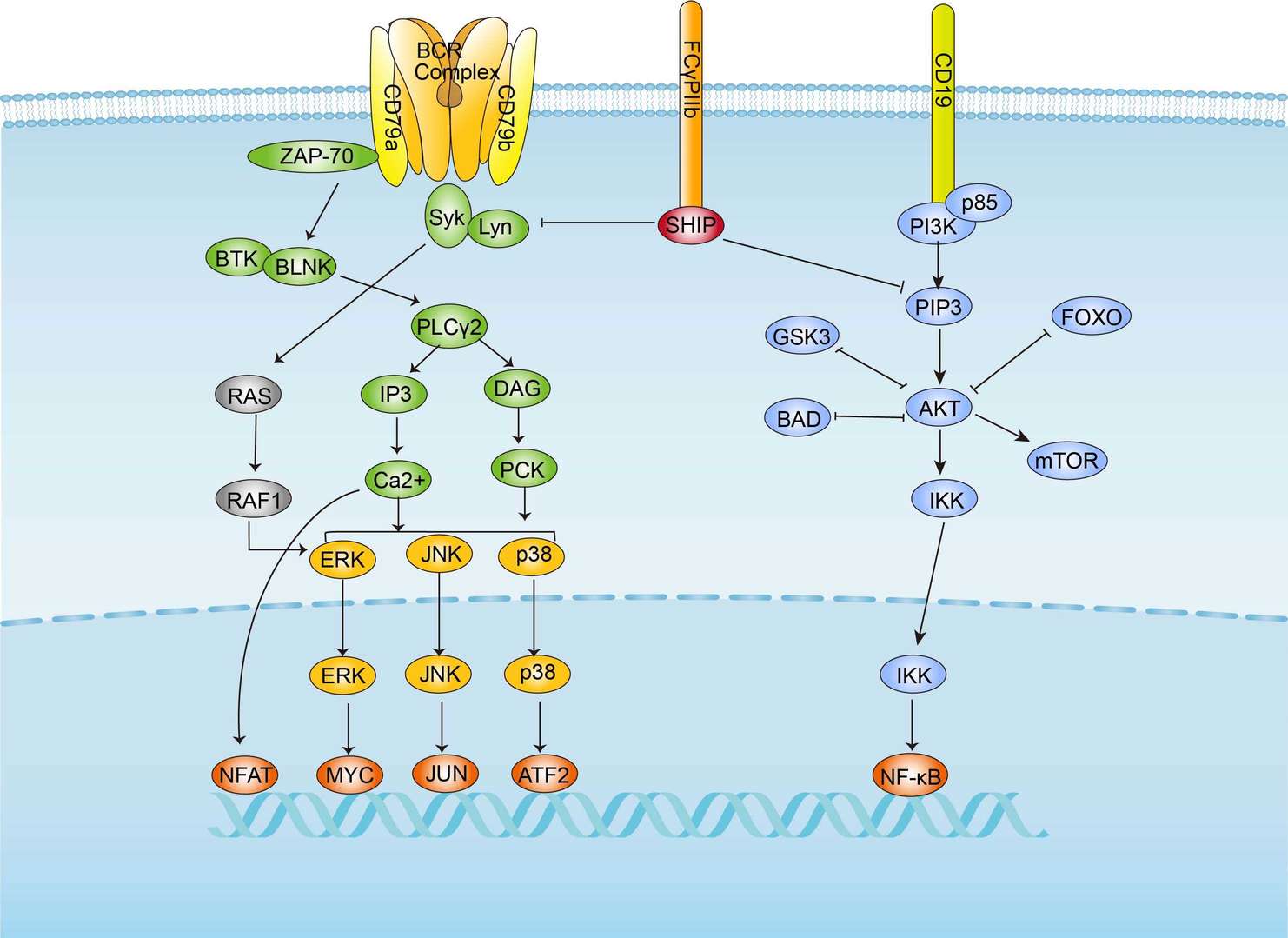 BCR Signaling Pathway
BCR Signaling Pathway